The World Alzheimer Report 2009 estimated that 36 million people worldwide are living with dementia, with numbers doubling every 20 years to 66 million by 2030, and 115 million by 2050. The majority of those individuals will have Alzheimer’s disease (AD).1
The rapid growth of AD cases worldwide, estimated by the National Institutes of Health (NIH) to be more than five million in the US alone, is approaching epidemic proportions and is threatening to overwhelm healthcare systems.
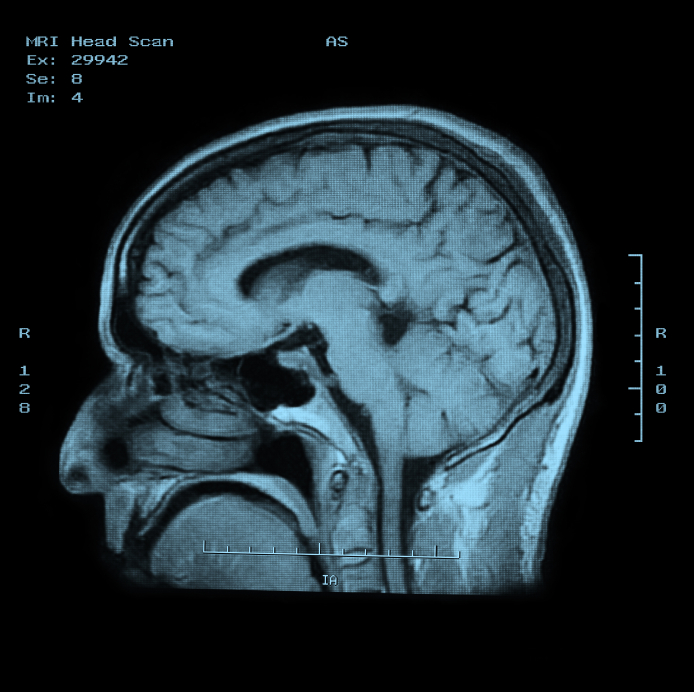
Definitive diagnosis of AD has traditionally relied upon post-mortem neuropathologic tissue analysis, requiring histological examination of brain tissue at autopsy, or in a rare case, following brain biopsy.2
Biomarkers are measurable proteins or genes in the body that relate to normal and abnormal processes within the body. In the case of AD, two biomarkers within the cerebrospinal fluid (CSF) can be measured to monitor Alzheimer’s disease progression—amyloid ß and tau proteins. It has been shown that the level of amyloid ß protein decreases during AD pathology.3
Conversely, the level of the tau protein increases as neuroaxonal degeneration progresses, and the level of hyper-phosphorylated tau protein goes up as tangle pathology occurs. While CSF biomarkers may provide accurate diagnostic information concerning the progression of the disease, the availability of samples for research studies and the practicality of their use for screening are limited by the invasiveness of the procedure required to collect the sample. Sample volume is also limited, and multiple spinal punctures are not an option. The most obvious alternative sample source is blood. However, Aß42 levels in CSF and plasma do not correlate, and tau is apparently present at concentrations too low to be useful.4 As a result, several efforts are under way to identify biomarkers in blood that can potentially be used to reliably diagnose AD.
A recent study published in Alzheimer’s & Dementia has identified a set of ten proteins in the blood that can potentially predict the onset of Alzheimer’s Disease. This test could be used for clinical trials of experimental treatments being developed to counter the development of AD. The research team used samples from three international studies: AddNeuroMed (ANM)—a multicenter European study, Kings Health Partners-Dementia Case Register (KHP-DCR)—a UK clinic and population based study, and Genetics AD Association (GenADA)—a multisite case-control study based in Canada. Samples from 1148 subjects, 476 with AD, 220 with MCI (mild cognitive impairment), and 452 elderly controls with no dementia were used in the study.
Seven Milliplex® MAP multiplex panels (96-well plate format; MilliporeSigma), based on Luminex xMAP® Technology, were utilized, and screened a total of 27 proteins that had been previously indicated as potential biomarkers of AD.
Ten proteins (TTR, Clusterin, cystatin C, A1AcidG, ICAM1, CC4, pigment epithelium-derived factor [PEDF], A1AT, RANTES, ApoC3) plus APOE were strongly associated with disease severity and disease progression.
Find out more about Luminex xMAP Technology and Alzheimer’s Disease research by downloading our free whitepaper: Four Ways Multiplexing Advances Alzheimer’s Disease Research.
References
- Prince M, Jackson J. World Alzheimer Report. Alzheimer’s Disease International: London, England, 2009.
- Rosen C, Hansson O, Blennow K, Zetterberg H. Fluid biomarkers in Alzheimer’s Disease—current concepts. Molecular Neurodegeneration 2013;8(U6 – U16).
- Hampel H, Shen Y, Walsh D, Aisen P, Shaw L, Zetterberg H, Trojanowski J, Blennow K. Biological markers of amyloid ß-related mechanisms in Alzheimer’s Disease. Experimental Neurology 2010;223(2):334-346.
- Zetterberg H, Blennow K. Cerebrospinal fluid biomarkers for Alzheimer’s Disease: More to come? Journal of Alzheimers Disease 2013;33(S361 – S369).