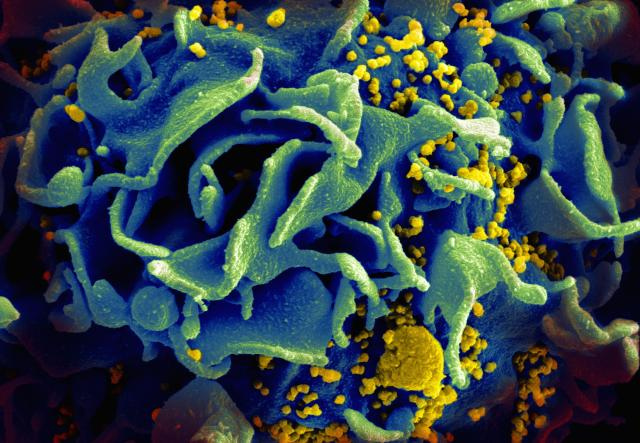
Scanning electromicrograph of an HIV-infected T cell. HIV Infected T cell by NIAID is licensed under Creative Commons License.
Human Immunodeficiency Virus (HIV) was first described 30 years ago, and in those 30 years, over 25 million people have died from it, according to the WHO. It continues to be a global challenge, although research and development teams have made great strides in treatment.
Countries with limited resources are particularly vulnerable to the disease, as HIV transmission is occurring quickly and access to healthcare is difficult. In addition, an emergence of a new form of HIV was inevitable—a form resistant to treatment, that will continue to mutate and reproduce within the presence of antiretroviral drugs (ARV).
In a new study published in the Journal of Clinical Microbiology,1 researchers have developed, tested, and validated a multiplex allele-specific (MAS) HIV subtype C drug resistance detection assay using Luminex’s suspension array system, MAGPIX®, and xMAP® and xTAG® Technology. (Learn more about developing your own assays.) This assay can simultaneously detect HIVDR mutations at 20 loci, and is faster, easier to use, more sensitive, and more cost-effective than the alternatives, such as sequencing or commercial genotyping assays.
Two types of assays have previously been developed to detect HIV drug resistance (HIVDR) mutations: sequencing-based and allele-specific assays. Sequencing-based assays are generally labor-intensive, and are not as sensitive as MAS assays when detecting low-abundance mutations. Allele-specific assays, while more sensitive than sequencing-based, can only detect a few mutations at a time.
In this study, the authors describe the developed assay in detail. It is not only a cost-effective solution, but it saves time—it can detect 45 alleles in a single reaction tube. This reduces the number of tubes/wells used for each sample test to just one, which allows for the genotyping of 96 or 384 samples in one plate, and it provides results in less than eight hours. The study also found that the MAS reliably detected Mut alleles at low levels of 1.56% to 12.5%, and 454 ultra-deep sequencing verified that more low-abundance alleles in specimens detected by the MAS assay.
The conclusions suggest that this assay could be an effective tool for HIVDR monitoring and surveillance on a large scale and in limited resource lab settings.
Luminex’s xMAP Technology is flexible and open-architecture, so it can be configured to perform a wide variety of assays. For detailed instructions on designing, creating, optimizing, and validating your own multiplex assays, download our free xMAP Cookbook.
References
- Zhang G, Cai F, Zhou Z, Devos J, Wagar N, Diallo K, Zulu I, Wadonda-Kabondo N, Stringer JS, Weidle PJ, Ndongmo CB, Sikazwe I, Sarr A, Kagoli M, Nkengasong J, Gao F, Yang C. Simultaneous detection of major Drug Resistance Mutations in the Protease and Reverse Transcriptase Genes for HIV-1 Subtype C by Use of a Multiplex Allele-Specific Assay. J Clin Microbiol 2013;51(11):3666-74. Available from: http://jcm.asm.org/content/51/11/3666.
